Case Study: Bridging the Gap in Patient-Physician Dialogue with Behavioural Science and Immersive Technology
The Challenge
Communication breakdowns between healthcare professionals (HCPs) and patients hinder effective care, especially for rare diseases like Myasthenia Gravis (MG). Traditional Continuing Medical Education (CME) often overlooks the behavioural and psychosocial dimensions of patient experiences, resulting in gaps in shared decision-making (SDM).
MG patients frequently report fluctuating symptoms, emotional isolation, and the need for constant adaptation. On the other hand, physicians struggle to connect these lived experiences with treatment strategies, creating a mismatch in communication and care priorities.
Our Approach: Behavioural Science Meets Immersive Learning
The ENGAGE project was originally initiated by Dr. Ina Weisshardt of LLH Concepts, a healthcare education and innovation consultancy focused on improving physician-patient dialogue. I was brought on board to lead the research design and analysis, working in collaboration with academic researchers from the University of Warwick.
ENGAGE was designed with behavioural concepts at its core, recognising that lasting changes in empathy, attitudes, and practices require more than education—they require understanding and influencing human behaviour.
Our three-phase approach integrated behavioural frameworks to address challenges systematically:
Phase 1: Needs Assessment
Conducted interviews and surveys using behavioural frameworks such as the Theoretical Domains Framework (TDF) to identify gaps in physician motivation, beliefs, and capabilities related to SDM.
55 physicians
133 patients
Phase 2: Educational Intervention
Leveraged Virtual Reality (VR) to simulate the daily life of an MG patient, emphasising not just physical symptoms (e.g., double vision, fatigue) but also the emotional and social challenges like stigma and isolation.
Incorporated behavioural insights into interactive workshops and debrief sessions to help physicians internalise these experiences and understand their practical implications for treatment.

Phase 3: Outcomes Evaluation
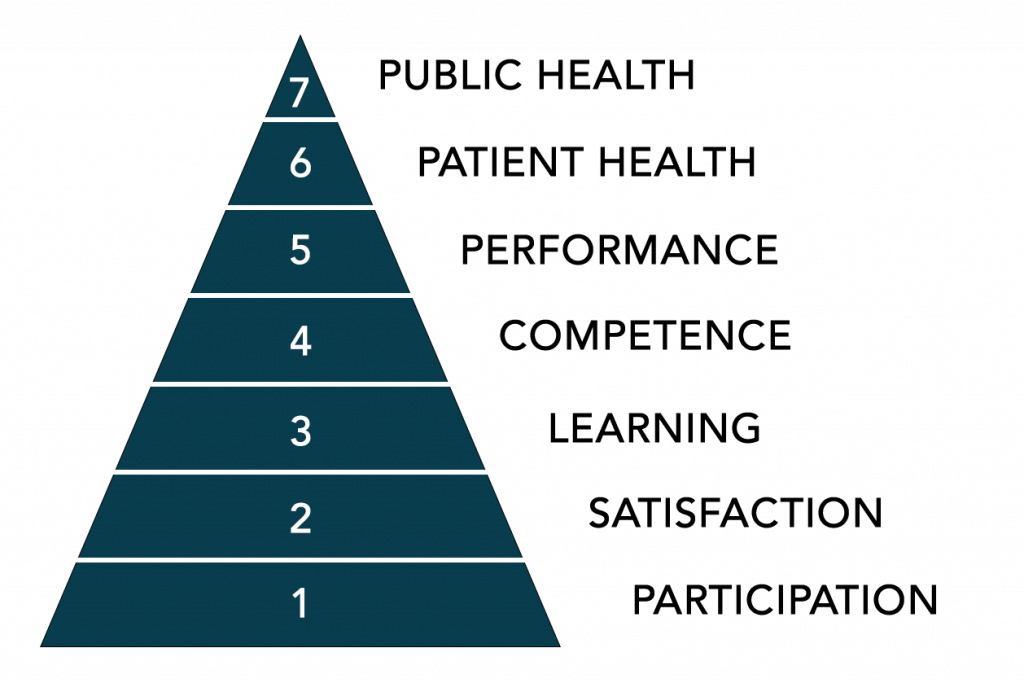
Applied the Moore Framework and TDF to measure shifts in attitudes, empathy, and behavioural intentions, ensuring that changes were tied to measurable behavioural constructs.
Results That Speak for Themselves
Empathy Boost
94% of physicians reported a deeper appreciation for the patient experience.
78% of participants expressed an increased intent to implement patient-centred practices.
Communication skills like active listening and sensitivity to patient values showed marked improvements, reflecting key shifts in beliefs about capabilities and social influences.
Post-intervention, TDF metrics highlighted significant gains in areas like motivation, behavioural regulation, and reinforcement, driving sustained improvements in shared decision-making practices.
The Impact
The ENGAGE project demonstrated the unique power of combining behavioural science principles with immersive technologies like VR to foster empathy and transform physician-patient interactions.
By focusing on behaviour change, this innovative programme enabled physicians to align treatments with patient values, improving both communication and care outcomes.
The intersection of behavioural science and immersive learning creates a powerful pathway to reimagine medical education, ensuring that patient voices are heard and integrated into care strategies.